Instruments Used in Birth: What They Do, When They’re Used, and Why Understanding Them Matters
pregnancy woman
Instrumental birth is one of the most poorly understood aspects of modern maternity care. For many parents, forceps or ventouse are only introduced at the point they are recommended — often during an intense, time-pressured moment.
Yet these tools have clear clinical indications, specific mechanical functions, and predictable implications for birth experience and recovery. Understanding them antenatally allows parents to engage with decisions from a place of knowledge rather than fear.
What Is an Instrumental Birth?
An instrumental (or assisted vaginal) birth occurs when tools are used to aid the baby’s descent through the birth canal during the second stage of labour.
In the UK, this typically involves:
Forceps
Ventouse (vacuum extraction)
These interventions are usually considered when:
The cervix is fully dilated
The baby’s head is low in the pelvis
Vaginal birth is still achievable
There is a clinical reason to expedite birth
Crucially, instrumental birth sits between spontaneous vaginal birth and caesarean section — often aiming to avoid major abdominal surgery when vaginal birth remains possible.
The Physiology Behind “Failure to Progress”
Before instruments are considered, clinicians assess why progress has slowed or stopped. This is not simply about time.
Factors influencing second-stage progress include:
Fetal position (e.g. occiput posterior or transverse)
Pelvic biomechanics
Maternal fatigue
Hormonal environment (oxytocin–adrenaline balance)
Pain, fear and sympathetic nervous system activation
Understanding this matters because:
Some causes are mechanical
Some are physiological
Some are environmental or emotional
Instrumental birth is often recommended when mechanical assistance is the most effective way to resolve the situation safely.
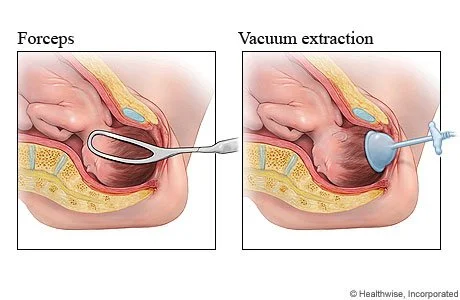
Image showing different types of instrument birth. Image from New York Presbytarian
Forceps: Mechanical Precision
Forceps are curved metal instruments designed to fit around the baby’s head. Their primary function is guided traction, sometimes combined with rotation.
Forceps may be recommended when:
The baby’s head needs to rotate to a more optimal position
There is a need for controlled, directional guidance
Immediate birth is required
From a technical standpoint, forceps allow the clinician to:
Apply traction in line with the pelvic curve
Assist rotation where needed
Deliver the baby in synchrony with contractions
Implications to understand
Higher association with perineal trauma
Can require episiotomy
Clear postpartum pelvic floor considerations
Typically very effective when used by skilled operators
Forceps are not “outdated” — they are highly skilled instruments, but outcomes depend heavily on practitioner expertise and context.
Ventouse: Traction Without Rotation
Ventouse (vacuum extraction) uses a suction cup applied to the baby’s scalp to assist descent during contractions.
Ventouse is usually chosen when:
The baby is already well-positioned
Rotation is not required
Assistance is needed to support expulsive efforts
From a mechanical perspective:
Traction is applied during contractions
The parent’s pushing remains central
Less space is taken within the pelvis compared to forceps
Implications to understand
Temporary scalp swelling (chignon) is common
Lower rates of severe perineal trauma compared to forceps
Less control over rotation
May fail, requiring escalation
Ventouse is often perceived as “gentler”, but it is not universally appropriate — the choice is context-specific, not hierarchical.
Decision-Making Under Pressure: Why Antenatal Knowledge Matters
Instrumental birth decisions are often made quickly, particularly where fetal wellbeing is a concern. In these moments, informed consent relies heavily on prior understanding and birth partners helping advocate for the birthing person.
Parents who have learned about instruments antenatally are more likely to:
Understand why assistance is being suggested
Ask relevant questions (“Why this instrument?”)
Feel involved rather than overridden
Process the experience more positively afterwards
Evidence consistently shows that perceived understanding and involvement correlate strongly with birth satisfaction — regardless of outcome.
Instruments and Postpartum Recovery
Instrumental birth can influence postpartum recovery in specific ways:
Increased pelvic floor loading
Greater likelihood of perineal trauma
Feeding challenges related to birth experience or infant discomfort
Emotional processing needs
These are not failures — they are predictable physiological consequences that benefit from early, informed support.
This is where postpartum feeding support, recovery care and birth debriefs become clinically relevant, not optional extras.
Processing Instrumental Birth Experiences
Many parents seek birth debriefs following instrumental birth to understand:
Why intervention was recommended
Whether alternatives were available
How physiology and circumstances interacted
What this means for future births
Debriefing is not about rewriting the past — it is about integrating experience, reducing self-blame and restoring confidence.
Why We Teach This as Part of Birth Preparation
At The Bubba & Me Club, we include detailed, evidence-based discussions of birth instruments within antenatal education because informed parents cope better — during birth and after.
Understanding instruments:
Does not make birth more intervention-heavy
Does not undermine trust in clinicians
Does not remove flexibility
Instead, it supports informed consent, emotional resilience and postpartum wellbeing.
Evidence-Based Antenatal Education and Birth Debriefs in Sevenoaks
At our Sevenoaks clinic, this approach is strengthened through our partnership with Professor Ranjit Akolekar, consultant obstetrician and fetal medicine specialist at The Pregnancy Clinic. Working alongside consultant-led medical care allows families to access clear clinical expertise alongside evidence-based antenatal education, birth preparation and postpartum support. This joined-up model ensures care is informed, coordinated and grounded in both medical science and physiological understanding.